Brain Tumors
Developmental Neurobiology and Pediatric Neuro-Oncology
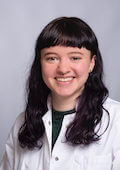
Schüller Research Group
Brain tumors account for the second most frequent type of cancer in childhood. To gain insight into how these tumors arise, it is essential to understand how the brain develops. The research projects of Prof. Dr. Ulrich Schüller's group at the interface of developmental neurobiology and neuro-oncology seek to understand, better detect and specifically treat pediatric brain tumors. The focus is on medulloblastomas, atypical teratoid/rhabdoid tumors (AT/RT) and spinal ependymomas. For this purpose, comprehensive morphological and molecular analyses of pediatric brain tumors are conducted, in vitro analyses are performed, and transgenic animal models are used.
Many tumors are known to exhibit pathological alterations within the SMARCA4 gene. In the field of pediatric neuro-oncology, this is especially true for rhabdoid tumors and medulloblastomas. For rhabdoid tumors, the Schüller research group has shown that tumors with SMARCA4 mutations represent a distinct subgroup that can be well differentiated clinically and molecularly from other rhabdoid tumors (see Holdhof et al. Acta Neuropathol 2021). Within medulloblastomas, such mutations have been most frequently reported in WNT medulloblastomas and group 3 medulloblastomas. However, the function of these alterations is often unknown. Thus, in a variety of ways, the researchers are elucidating what role SMARCA4 plays in the development of the nervous system (see e.g. Holdhof et al., Development 2021) and in the pathogenesis of tumors of the nervous system. In doing so, they aim to find out when, where, and how a functionally intact SMARCA4 is required for brain development, how a pathologically altered SMARCA4 can initiate or accelerate tumor development, whether it contributes to metastasis and/or is associated with more aggressive tumor growth, and to what extent SMARCA4 can play a role as a potential target for anticancer therapy.
Atypical teratoid/rhabdoid tumors (AT/RT) are rare, highly aggressive tumors that occur in the spinal cord and brain. The exact cellular origin of these tumors is still not entirely clear, even though the Schüller group has already made relevant contributions to this topic (see e.g. Moreno et al. J Neurosci 2014; Graf et al. Nat Commun, 2022). Rhabdoid tumors usually occur in the first twelve months of a child's life. They are caused by mutations in two different genes, SMARCA4 and SMARCB1. The prognosis for these young patients is particularly poor if the tumor recurs or even metastasizes. At this point, very few treatment options are available because the mechanisms leading to recurrence or metastasis are largely unknown. Therefore, the research group is conducting intensive research to understand which characteristics distinguish recurrent tumors from primary tumors.
The scientists are working at the genetic, epigenetic and transcriptional level to functionally validate mutations specific to recurrent tumors and to test – both in vitro and potentially also in vivo – how such changes are suitable as anticancer drug targets.
Ependymomas are tumors of the central nervous system, some of which grow very aggressively. They arise from degenerated cells of the brain or spinal cord. While intracranial tumors occur mainly in childhood, spinal ependymomas are seen mainly in adulthood, unless neurofibromatosis is present, which can be associated with such spinal tumors at an early age (see, e.g., Kresbach et al., Acta Neuropathol 2021; Kresbach et al., Brain Pathol 2022). The research group is currently working intensively on the correlation of morphological and molecular characteristics with the clinical course of these diseases. In doing so, the researchers are also focusing on the inter- and intratumoral heterogeneity of the tumors, the clinical significance of which has received little attention to date. The methods used include global methylome analyses and DNA and RNA sequencing, which may even be performed at the single cell level or spatially resolved (scSeq or spatial omics analysis).
Until now, precise molecular diagnostics of brain tumors has required the analysis of tissue samples taken by neurosurgery. To complement tissue-based diagnostics, we use Nanopore sequencing to characterize cell-free DNA in CSF samples. This allows us to determine copy number profiles and the global methylome, to match the corresponding features of the DNA with large databases, and to make an accurate molecular classification of the tumor. This enables us to diagnose brain tumors, for which a tissue biopsy is very or too risky. In addition, surgical interventions can be planned more individually in view of a known molecular diagnosis, and residual disease and recurrences can be detected easily and at an early stage. In the medium term, the technology will be implemented in clinical trials to randomize patients based on molecular CSF diagnostic results.
Medulloblastomas are metastatic pediatric tumors from which, despite a relatively good understanding of the disease, many patients still die. The Schüller group was able to make important contributions to understanding where and how exactly these tumors arise (see e.g. Schüller et al. Cancer Cell 2008; Grammel et al., Acta Neuropathol 2012; Merk et al., Dev Cell 2018). Also, inhibitors of the Sonic hedgehog (SHH) signaling pathway have already been used successfully to combat tumors. However, because unacceptable systemic side effects of these inhibitors have been observed in children, we are currently working on novel local therapeutic approaches in the form of intraventricular drug applications. This also involves the use of transgenic animal models previously developed by the researchers. In addition, they are trying to find additional ways to slow the growth of SHH medulloblastomas with immunological approaches targeting the EGFR protein. Such new approaches are particularly important in very young children who cannot be irradiated and in whom the SHH subtype of medulloblastoma is particularly common.
Malignant gliomas are among the most malignant tumors of childhood. As an alternative to H3F3A hotspot mutations, MYCN amplifications are known as tumor-driving genetic alterations. MYCN amplified gliomas, which also have TP53 mutations in approximately 60 % of cases, show clearly delineated patterns of global DNA methylation and gene expression and are also clinically distinct from other childhood brain tumor entities. In preliminary work, the scientists have generated hGFAP-cre::lox-STOP-loxMYCN,p53Fl/Fl mice that develop malignant gliomas with overexpression of MYCN and loss of p53. They are now using this model to better understand the biology and treatment options of MYCN amplified malignant gliomas. First, the temporal and cellular origin of the tumors will be elucidated. Next, the local growth behavior, tumor spread and independent growth will be studied in vitro and in vivo. Then they will analyze morphologically and molecularly to what extent murine and human tumors are comparable before in a final step pursuing first targeted therapeutic approaches.
After studying medicine in Freiburg, Bonn and Munich, Ulrich Schüller received his doctorate in medicine from the University of Bonn in 2003. He began his medical career at the Institute of Neuropathology at the University of Bonn before conducting research at the Dana-Farber Cancer Institute at Harvard University in Boston from 2005-2006 on a grant from German Cancer Aid. His main research interest has always been the development of the nervous system and the pathogenesis of pediatric brain tumors. In 2007, he continued his residency training as a neuropathologist at the Center for Neuropathology at the University of Munich, where he established his own research group as part of the Max Eder Junior Research Group Program of German Cancer Aid.
This was followed by his board certification in 2009 and his Habilitation, venia legendi and appointment as senior physician in 2010 in Munich. After declining the offers of professorships from the Universities of Würzburg and Lausanne, in 2016 Ulrich Schüller accepted a professorship in molecular pediatric neuro-oncology at the University Medical Center Hamburg-Eppendorf (UKE), where he works as a senior physician at the Institute of Neuropathology in addition to his scientific activities at the Research Institute Children's Cancer Center Hamburg. There, he is primarily responsible for the diagnosis of pediatric brain tumors and molecular neuropathology. He acts as reference neuropathologist for the SIOP Ependymoma II study for the treatment of children with ependymomas and runs the UKE core facility for global methylome analyses.
Deutsche Forschungsgemeinschaft (DFG)
Deutsche Krebshilfe
Deutsche Kinderkrebsstiftung
FightKidsCancer
Tour der Hoffnung
Rüdiger Colditz Stiftung
Schoof M, Godbole S, Albert T, Dottermusch M, Walter C, Ballast A, Qin N, Baca Olivera M, Göbel C, Neyazi S, Holdhof D, Kresbach C, Peter L, Epplen D, Thaden V, Blattner-Johnson M, Modemann F, Mynarek M, Rutkowski S, Sill M, Varghese J, Afflerbach A, Eckhardt A, Münter D, Struve N, Jones D, Remke M, Neumann J, Kerl K, Schüller U. Mouse models of pediatric high-grade gliomas with MYCN amplification reveal intratumoral heterogeneity and lineage signatures. Nat Commun 2023, 14(1):7717.
Holdhof D, Schoof M, Al-Kershi S, Spohn M, Kresbach C, Göbel C, Hellwig M, Indenbirken D, Moreno N, Kerl K, Schüller U. Brahma-related gene 1 has time-specific roles during brain and eye development. Developement. 2021;148(10):dev196147.
Merk D, Ohli J, Merk N, Thatikonda V, Morrissy S, Schoof M, Schmid S, Harrison L, Filser S, Ahlfeld J, Erkek S, Raithatha K, Andreska T, Weißhaar M, Launspach M, Neumann J, Shakarami M, Plenker D, Marra M, Li Y, Mungall A, Moore R, Ma Y, Jones S, Lutz B, Ertl-Wagner B, Rossi A, Wagener R, Siebert R, Jung A, Eberhart C, Lach B, Sendtner M, Pfister S, Taylor M, Chavez L, Kool M, Schüller U. Opposing effects of CREBBP mutations govern the phenotype of Rubinstein-Taybi syndrome and adult SHH medulloblastoma. Dev Cell, 2018. 44, 709–724.
Neumann J, Wefers A, Lambo S., Bianchi E, Bockstaller M, Dorostkar M, Meister V, Schindler P, Korshunov A, von Hoff K, Nowak J, Warmuth-Metz M, Schneider M, Müller-Renner I, Merk D, Shakarami M, Sharma T, Chavez L, Glass R, Chan J, Taketo M, Neumann P, Kool M, Schüller U. A mouse model for Embryonal Tumors with Multilayered Rosettes (ETMRs) predicts tumor responsiveness to Sonic hedgehog inhibitors. Nat Med. 2017; 23(10):1191-1202
Schüller U, Heine V, Mao J, Kho AT, Dillon AK, Han YG, Huillard E, Sun T, Ligon AH, Qian Y, Ma Q, Alvarez-Buylla A, McMahon A, Rowitch DH, Ligon KL. Acquisition of granule neuron precursor identity is a critical determinant of progenitor cell competence to form Hedgehog-induced medulloblastoma. Cancer Cell. 2008; 14: 123-134.
Gesamtverzeichnis der Publikationen: Pubmed












New approaches in the diagnosis of childhood brain tumors
Patients´ Story